Trigeminal Neuralgia is medically recognized as the most severe and unbearable pain of the face. Patients often describe this pain as “like a knife stabbing into our face suddenly,” “an instant and very sharp pain like an electric shock.”
A simple speaking movement, a bite of food, brushing teeth, washing the face, or even just a light breeze touching your face can trigger these sudden pain attacks. For this reason, people can often avoid touching their faces, speaking, and even laughing.
Trigeminal Neuralgia pain may not be recognized in the early period. Unfortunately, this disease is often misinterpreted. Patients can be mistaken for sinusitis for months or even years, have teeth extracted incorrectly, and be subjected to useless and risky procedures such as unnecessary root canal treatments and sinus surgeries.
This situation not only delays treatment but also seriously reduces the patient’s quality of life. Since this disease comes with aggressive and unexpected attacks, it can seriously affect both social life and psychological state. However, with timely diagnosis and expert management, pain can be controlled and quality of life can be significantly improved. Trigeminal Neuralgia is a disease that can be effectively treated when correctly diagnosed; therefore, it is vital for people experiencing severe facial pain to consult a neurology specialist early.
What is Trigeminal Neuralgia?
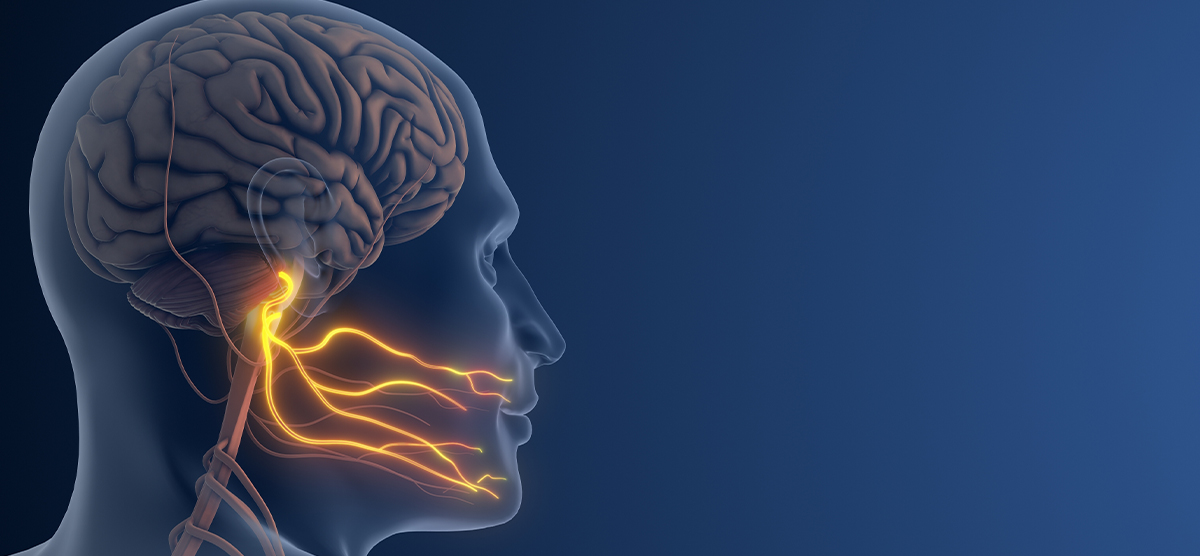
Trigeminal Neuralgia is a severe facial pain disease characterized by attacks resulting from the involvement of the 5th cranial nerve (trigeminal nerve) that carries sensations in our face.
This nerve divides into three main branches:
- V1 (Ophthalmic branch): Forehead and eye area
- V2 (Maxillary branch): Cheek, upper teeth, upper jaw
- V3 (Mandibular branch): Lower jaw, lower teeth, lip and chin area
Trigeminal Neuralgia most commonly affects V2 and V3 regions, namely the cheek, upper and lower jaw areas of the face.
Patients describe the pain as electric shock-like, sharp like a knife stabbing, or burning like flames. In trigeminal neuralgia, sudden, severe, recurrent attacks lasting several seconds reduce the patient’s quality of life.
The pain is so severe that:
- Speaking
- Brushing teeth
- Shaving
- Eating
- Touching the face
- Wind blowing
even the slightest contact can trigger a new attack.
Fear and anxiety increase in some patients because when the pain will come is unpredictable.
What Causes Trigeminal Neuralgia?
The most common cause of Trigeminal Neuralgia is a blood vessel pressing on the nerve in the area near the brainstem of the trigeminal nerve. This pressure gradually damages the protective sheath of the nerve (myelin layer) and the nerve literally begins to send false and excessive pain signals like an electric cable with stripped insulation.
However, this is not the only cause. Trigeminal Neuralgia can occur due to many different reasons:
Neurovascular Compression (Most Common Cause)
- Damage to the nerve occurs as a result of compression of the trigeminal nerve by an artery or vein.
- Usually seen in advanced age and is called primary trigeminal neuralgia.
Multiple Sclerosis (MS)
- It is the most important cause of trigeminal neuralgia in young patients.
- MS causes attack-type pain by directly affecting the myelin layer of the nerve.
Tumors and Masses
- Tumors or cysts around the brainstem can compress the trigeminal nerve.
- In newly emerging, progressively worsening facial pains, evaluation of the trigeminal nerve with brain Magnetic Resonance (MR) Imaging is absolutely necessary.
Infections
- Post-herpetic neuralgia can develop especially after Shingles (Herpes Zoster).
- Viral/bacterial infections in the facial region can damage the trigeminal nerve.
Degenerative and Vascular Stiffness Processes
- Stiffening in vascular structures and blood flow changes with age
- Deterioration in nerve nutrition causing myelin damage can prepare the ground for trigeminal neuralgia development by irritating the trigeminal nerve.
Anatomical Variations (Congenital Structural Proximity)
- The risk of compression is higher in people whose nerves and vessels run closer than normal.
Trauma and Surgical Procedures
- Blows to the facial region
- Tooth extractions, facial surgeries
- Incorrect application of fillings or botox can cause damage to trigeminal nerve fibers.
Connective Tissue and Inflammatory Diseases
- Inflammation and compression can develop around the trigeminal nerve in diseases such as rheumatoid arthritis, Sjögren’s syndrome, etc.
What Situation is Alarming?
Severe facial pain starting at a young age
New pain starting suddenly that has never been experienced before
Gradual worsening of pain or weakness in facial muscles
In this case, it is necessary to consult a neurology specialist.
What Are the Symptoms of Trigeminal Neuralgia?
The symptoms of Trigeminal Neuralgia are quite characteristic and easily noticed by patients. The pain can be so sharp and sudden that the person may freeze and become unable to move.
Severe Facial Pain Starting Suddenly Like an Electric Shock
- Pain can last seconds to minutes.
- Described as knife stabbing, lightning striking, burning, or needle-like.
- Intensity can be described as 10 out of 10.
Unilateral Pain Always on the Same Side
- Usually seen on one side of the face and does not switch sides.
- Occurrence on both sides simultaneously suggests secondary causes → neurology evaluation is definitely required.
Pain Attacks Triggered by Trigger Points
Even simple stimuli can start an attack:
- Brushing teeth
- Chewing, talking, swallowing
- Washing face, applying makeup
- Shaving
- Light touch, stroking the face
- Wind blowing or cold air contact
This feature is one of the most critical findings in diagnosis.
Completely Pain-Free Periods Between Attacks
- The face is completely normal in between.
- This distinguishes it from other chronic facial pains.
Pain Localized to Specific Facial Areas
Pain is most commonly felt in the area of the lower two branches of the trigeminal nerve (V2-V3):
- Pain radiating from cheek to jaw
- Lip, gums, tooth root area
- Sometimes eye and temple area
Alarm Signs
Secondary trigeminal neuralgia is considered in the following situations:
– Bilateral pain
– Continuous, never-disappearing pain
– Numbness, weakness in the face
In this case, urgent neurological evaluation is required.
In summary;
– Sudden and electric shock-like
– Unilateral and recurring in the same place
– Starting with simple triggers
– Attacks occurring in episodes are typical for Trigeminal Neuralgia.
International Classification of Headache Disorders (ICHD-3) Diagnostic Criteria – 13.1 Pain attributed to a lesion or disease of the trigeminal nerve
- There must be unilateral recurrent paroxysmal facial pain attacks in the distribution of one or more branches of the trigeminal nerve and the pain should not extend beyond these areas. Additionally, criteria B and C must be met
- Pain has all of the following characteristics:
- Attacks lasting from a fraction of a second to 2 minutes
- Severe intensity
- Electric shock-like, shooting, stabbing, or sharp in quality
- Can be triggered by innocuous stimuli within the affected trigeminal distribution (e.g., washing face, brushing teeth, shaving, light touch)
- Pain cannot be better explained by another ICHD-3 diagnosis
Explanatory Notes
- If pain spreads outside the trigeminal nerve region, a different diagnosis should be considered.
- Attack durations are quite short; attacks can cluster consecutively.
- Patients generally describe the pain as “unbearable.”
- Triggered by mild stimuli that activate mechanoreceptors (allodynia-like).
Trigeminal Neuralgia Subtypes (ICHD-3)
Trigeminal neuralgia is divided into three main subtypes according to underlying causes. Classical (primary) trigeminal neuralgia occurs as a result of compression of the trigeminal nerve root usually by a vessel, and neurovascular contact can be seen on imaging methods. Secondary trigeminal neuralgia develops when a structural or disease-related cause such as multiple sclerosis, tumor, cyst, or previous trauma affects the trigeminal nerve. Painful trigeminal neuropathy is a condition where there is significant structural damage to the trigeminal nerve and neuropathic pain is predominant; in this form, pain may be more continuous and burning in character rather than paroxysmal attacks.
How is Trigeminal Neuralgia Diagnosed?
The diagnosis of Trigeminal Neuralgia is made through a detailed evaluation by a neurology specialist. Because the disease can often be confused with other facial pains, and accurate diagnosis is critically important for treatment success.
Detailed Medical History (Anamnesis)
Your doctor will ask you many questions about the pain.
- Duration and severity of pain
- Is it electric shock-like?
- Unilateral? Always in the same area?
- What situations trigger it? (tooth brushing, chewing, etc.)
- Are there completely pain-free periods between attacks?
These questions reveal the presence of typical signs for Trigeminal Neuralgia.
Neurological Examination
- Is there sensory loss or numbness in the face?
- Is the blink reflex normal?
- Is there weakness in the chewing muscles?
- Does touching trigger areas cause pain?
Examination is very important in understanding that there is no other underlying disease, i.e., that secondary causes are not causing the pain. If there are neurological examination findings accompanying the pain, detailed further tests must definitely be performed.
Magnetic Resonance Imaging (MRI)
It is the gold standard in diagnosis. Especially:
– Contact and compression between nerve and vessel
– Tumor, cyst, or vascular anomaly
– Brain MRI examination is very valuable in recognizing Multiple Sclerosis plaques.
MRI helps determine whether it is primary or secondary trigeminal neuralgia.
Note: High-resolution MRI techniques such as “FIESTA – CISS” are especially preferred.
Differential Diagnosis from Other Facial Pains
Conditions that need to be distinguished:
- Dental problems
- Cluster headache
- Sinusitis
- Temporomandibular joint disorder (TMD/TMJ)
- Giant cell arteritis
- Post-herpetic neuralgia
These diseases must be evaluated to prevent misdiagnosis.
Trigeminal Neuralgia Treatment
The goal in treating Trigeminal Neuralgia is to suppress the pain signals of the hypersensitive trigeminal nerve and improve the patient’s quality of life. Treatment is personalized according to the patient’s age, frequency of pain, and accompanying diseases.
Drug Treatment (First-Line Treatment)
Drug treatment is usually very effective in Trigeminal Neuralgia and is the first preferred method.
Antiepileptic (Neuropathic pain medications)
- Carbamazepine → Gold standard (provides significant relief in 80-90% of patients)
- Oxcarbazepine → Better tolerated, alternative to carbamazepine
- Gabapentin, Pregabalin → Especially effective in patients with widespread pain
- Lamotrigine, Baclofen → Supportive therapy in resistant cases
These medications should be used regularly; they should not be stopped suddenly.
Local Treatments
- Creams/sprays containing lidocaine can provide relief at trigger points in the facial area.
Surgical and Interventional Treatments
Evaluated when medications are insufficient or side effects cannot be tolerated.
Microvascular Decompression Surgery (MVD)
- It is the method with the highest permanent effect potential where the vessel compressing the nerve is removed.
- The most suitable option for young and healthy patients
Interventional Procedures
Can be done on an outpatient basis, in a short time:
| Method | Mechanism of Action |
| Radiofrequency Thermocoagulation | Reduces pain by controlled burning of nerve fibers |
| Balloon Compression | Prevents pain transmission by mechanically compressing the nerve |
| Glycerol Rhizolysis | Nerve is partially disabled with chemical substance |
Advantage: Rapid effect
Disadvantage: Risk of recurrence is higher compared to surgery.
Radiosurgery (Gamma Knife)
- Without opening the skull, the nerve root is intervened with focused radiation.
- Ideal for patients with high surgical risk or elderly patients
Precautions in Daily Life
These recommendations support treatment:
- Protect your face from cold, wind, and sudden weather changes
- Avoid very hot/very cold foods
- Prefer soft-textured foods
- Use a soft toothbrush and perform oral care gently
- Avoid sudden facial movements
- Apply stress management techniques (breathing exercises, relaxation techniques)
- Pay attention to sleep pattern
- Get psychological support if needed
(Trigeminal Neuralgia can cause anxiety and depression)
In summary,
– Trigeminal Neuralgia is a treatable disease.
– With appropriate drug treatment, pain is controlled in most patients.
– Surgical treatment options offer strong alternatives for patients who do not benefit from medications.
If you have pain, it is very important to consult a neurology specialist without delay.
Frequently Asked Questions About Trigeminal Neuralgia
1. Can Trigeminal Neuralgia Be Treated? Does It Completely Heal?
Yes, Trigeminal Neuralgia is a disease that can be largely controlled with proper treatment. Drug treatment significantly reduces pain in approximately 80-90% of patients.
However, complete recovery may vary from person to person:
- Pain can be controlled for a long time with drug treatment.
- Surgical methods such as microvascular decompression can provide resolution in suitable patients.
- Early diagnosis increases treatment success and quality of life
Personalizing treatment is critically important.
2. How is Trigeminal Neuralgia Distinguished from Toothache?
Trigeminal Neuralgia is a nerve-originated pain disease most commonly confused with dental problems. For accurate diagnosis, attention should be paid to the following differences:
| Characteristic Feature | Trigeminal Neuralgia | Toothache |
| Pain type | Electric shock-like, stabbing | Throbbing, continuous |
| Duration | Seconds-minutes | Hours-days |
| Triggers | Touch, speech, chewing, face washing | Cold-hot, chewing |
| Pain intervals | Completely pain-free periods | Shows continuity |
| Dental examination | Normal findings | Decay/infection may be visible |
If the dentist finds no problem, you should definitely consult a neurology specialist without unnecessary interventions.
3. Is Trigeminal Neuralgia Hereditary? If It’s in the Family, Will It Pass to My Child?
Generally, Trigeminal Neuralgia is not a hereditary disease. Most patients are the first to have it in the family.
However, in some cases, the risk may increase at a minimal level:
- Presence of Multiple Sclerosis (MS)
- Facial nerve compression due to vascular structure
- Connective tissue diseases
Even with family history, the likelihood of occurrence in children is extremely low.
4. Does Trigeminal Neuralgia Go Away on Its Own? Does It Last a Lifetime?
The course of the disease is individual:
- In some patients, attacks may disappear periodically
- In some, it can continue for years if not treated
- Age, stress, and fatigue can increase pain attacks
Good news:
– With appropriate drug treatment, most patients return to normal life
– Long-term recovery can be achieved with surgical options
Early application is important as the intensity of pain may increase as treatment is delayed.
5. Which Doctor Should I See If I Suspect Trigeminal Neuralgia?
The most appropriate application is to a Neurology Specialist.
The following specialties can contribute to the process:
- Neurosurgery → in cases requiring surgery
- Pain Clinic → for interventional treatments
- Family Physician → for initial evaluation and referral
Common mistakes:
- Unnecessary tooth extractions
- Futile sinus surgeries
- Just delaying with painkillers
Trigeminal Neuralgia is a neurological disease requiring special knowledge. Consulting a neurology specialist speeds up diagnosis and prevents unnecessary procedures.
6. Can Trigeminal Neuralgia Occur After Tooth Extraction or Sinus Surgery?
Yes. Trigeminal Neuralgia can sometimes occur after procedures such as tooth extraction, implant procedures, facial trauma, or sinus surgery. The reason for this is that trigeminal nerve branches pass through these areas and nerve fibers are affected during the procedure.
This situation is usually noticed as follows:
- After tooth extraction, pain intensifies instead of passing
- Pain spreads along the nerve pathway, not the tooth
- Short-duration attacks like electric shocks develop
- Dental examination and X-ray show everything is normal
- Despite repeated procedures in the same tooth area, pain does not improve
For this reason, patients can often be subjected to unnecessary treatments:
- Unnecessary multiple tooth extractions
- Mistaken root canal treatments
- Sinus surgeries when there is no need at all
If the pain character has changed after dental treatment and electric shock-like attacks have developed, consulting a neurology specialist without delay is necessary.
Of course! Here is an explanatory Q&A section prepared SEO-friendly in the way patients frequently ask:
7. Can Trigeminal Neuralgia Still Exist If MRI Comes Out Normal?
Yes, it can. A normal MRI does not rule out the diagnosis of Trigeminal Neuralgia. Because MRI may not always be sensitive enough to show the vessel compressing the nerve or the nerve damage.
This situation is more common especially in these groups:
- In the early period of the disease
- In cases where compression is at a microscopic level
- If the resolution of the imaging device is low
- In functional (non-secondary) trigeminal neuralgias
Diagnosis is made with history and clinical examination.
MRI is only used to rule out underlying serious causes (tumor, mass, vascular anomaly).
In summary:
Even if MRI is normal, if there is short-duration electric shock-like facial pain, Trigeminal Neuralgia is most likely correct.
Therefore, even if your MRI comes out normal:
- Do not resort to unnecessary dental treatments
- If pain persists, neurology specialist follow-up is definitely necessary

 Türkçe
Türkçe